Dental cellulitis, also known as facial cellulitis or odontogenic cellulitis, is a type of cellulitis that originates from an infection in the mouth or teeth. It occurs when bacteria from a dental infection spread to the surrounding tissues, causing inflammation and infection.
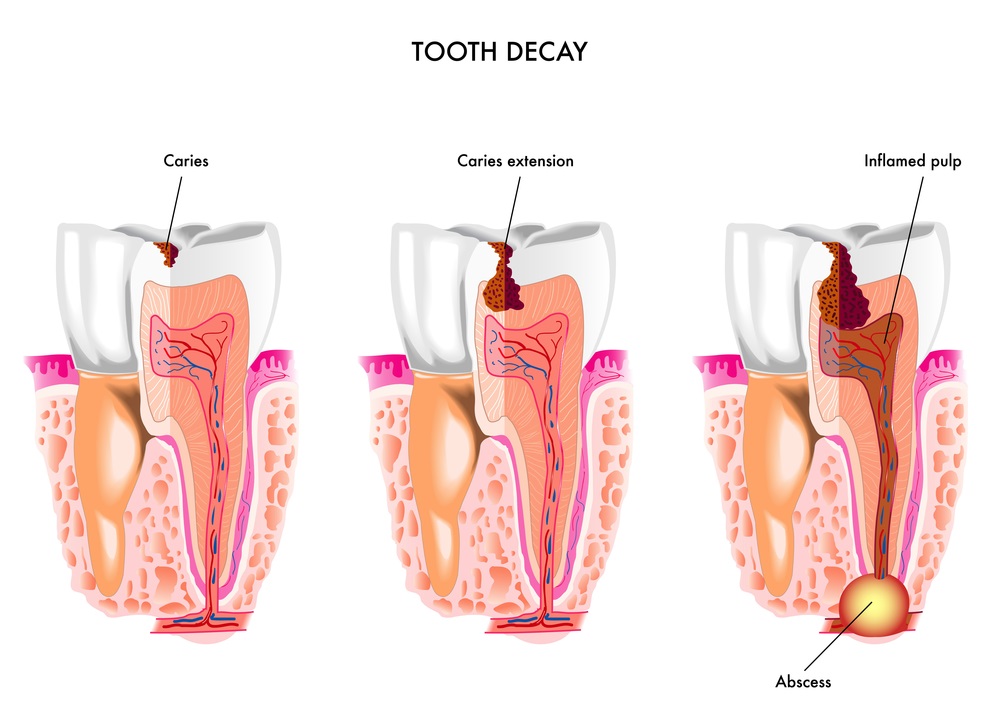
Dental cellulitis typically develops as a complication of untreated dental problems such as tooth decay, gum disease (periodontitis), or dental abscesses. These conditions can allow bacteria to enter the soft tissues of the face and neck, leading to cellulitis.
Causes: Dental cellulitis typically occurs when bacteria from a dental infection, such as a tooth abscess or periodontal disease, spread to the surrounding soft tissues. Poor oral hygiene, dental trauma, dental procedures, and systemic conditions that weaken the immune system can all contribute to the development of dental infections.
Risk Factors: Certain factors may increase the risk of developing dental cellulitis, including:
- Poor oral hygiene habits
- Dental cavities (caries)
- Gum disease (periodontal disease)
- Weakened immune system due to conditions like diabetes, HIV/AIDS, or chemotherapy
Symptoms: Symptoms of dental cellulitis can vary but often include:
- Swelling, tenderness, and redness in the face, neck, or jaw area
- Pain or discomfort, which may be localized to the affected tooth or gum area
- Fever and general malaise
- Difficulty swallowing or opening the mouth fully in severe cases
Diagnosis: A dentist can usually diagnose dental cellulitis based on a physical examination and review of symptoms. They may also use imaging tests such as dental X-rays or CT scans to assess the extent of the infection and identify any underlying dental issues.
Treatment: Treatment for dental cellulitis typically involves a combination of antibiotics and dental procedures to address the underlying infection. Antibiotics are prescribed to eliminate the bacterial infection, while dental treatment such as root canal therapy, tooth extraction, or incision and drainage of abscesses may be necessary to remove the source of infection. Pain relievers may also be prescribed to manage discomfort.
Complications: Without prompt treatment, dental cellulitis can lead to serious complications, including the spread of infection to other parts of the body, such as the brain or bloodstream (sepsis). In severe cases, it can also cause tissue damage, abscess formation, or even life-threatening conditions.
Prevention: Practicing good oral hygiene, including regular brushing and flossing, and scheduling routine dental check-ups can help prevent dental problems that may lead to cellulitis. Prompt treatment of dental issues such as cavities or gum disease can also reduce the risk of developing dental cellulitis.
If you suspect you have dental cellulitis or any other dental infection, it’s essential to seek prompt evaluation and treatment from a dentist to prevent complications and promote oral health.